BFIRST Trustee visit to Gaza
04 February 2026
(Last updated: 4 Feb 2026 16:41)
Dec 2025 Gaza Cleft Surgery
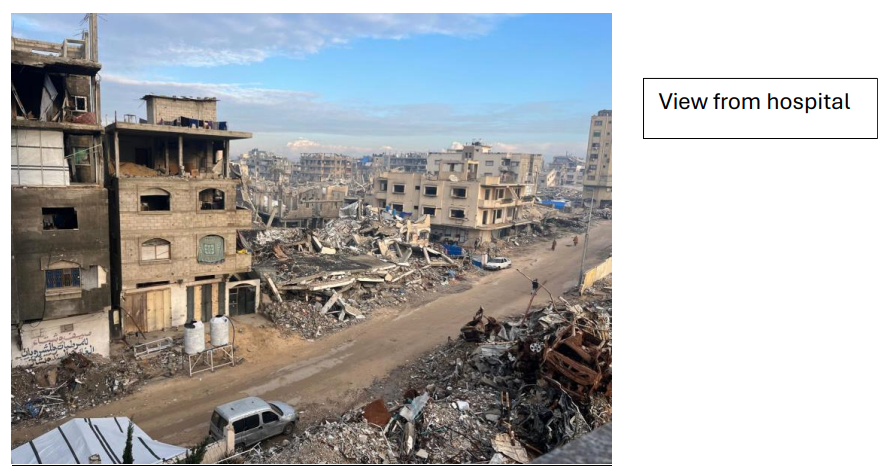
Mr Khurram Khan, Consultant Cleft & Plastic Surgeon and BFIRST Member visited Al-Shifa Hospital in December 2025 for 2 weeks. The travel was through a WHO registered charity organisation (Heroic Hearts, USA) with a well-established framework and local team in the region. The purpose of the trip was to focus on re-starting cleft surgery for the local population.
Preparatory work
This was carried out in the weeks and months leading up to the December trip.
- Multiple meetings with Mr Ahmed Mokhallati – Plastic Surgeon in the UK. Ahmed worked for 2 years in Gaza prior to the current conflict, performing cleft surgery locally and with a detailed understanding of the local health system and current links to the local plastic surgeons
- Identified and virtually met senior local Plastic surgeon, Dr Bassam Al-Masri.
- Al Shifa Hospital, north Gaza identified as potential base and proposed centre for Cleft Surgery going forwards
- Met and co-ordinated with the Gaza Infant Nutrition Alliance (GINA). This is a UK based charity with a local team in managing and monitoring infant nutrition. GINA has cleft children (primary, unrepaired) identified and prepped those with no clinical malnutrition for potential surgery
- Volunteer UK-based specialist Cleft speech therapist identified to provide remote/virtual support. Advice leaflets translated to Arabic.
Aims
- Assess local Cleft Surgery situation
- Establish relationship with identified local surgeons and team to train, teach and support high quality and safe local primary cleft surgery
- Start the process of building links for a locally based Cleft MDT, with virtual and/or visiting support from the UK
Overview of time spent
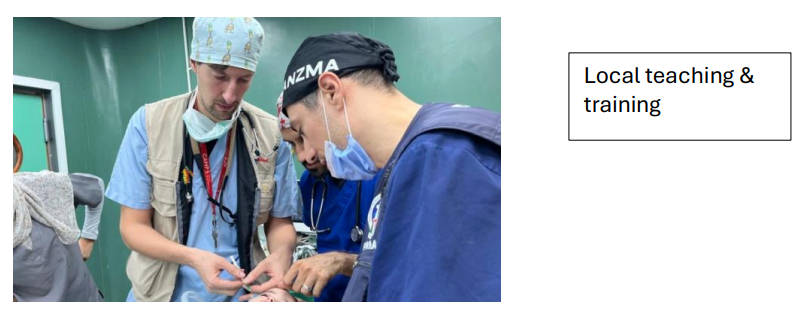
- Met with 5 out of 6 of the current local Plastic Surgeons in Gaza. Performed cases with and trained with 4 of these surgeons (2 identified as leads for cleft surgery)
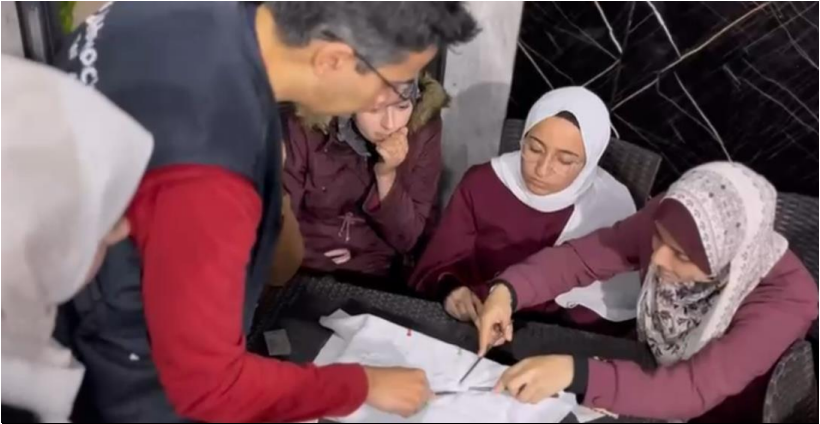
- Cleft Outpatient clinics x2 at Shifa Hospital
- Local doctor from GINA attended to support nutrition pre-post surgery
- UK cleft speech therapist sent patient speech sample videos to assess virtually and advise on surgical benefit
- Operated on 19 cases (17 cleft, 2 non-cleft complex nasal reconstructions)
- Majority unrepaired primary cleft palates
- Any children/infants only operated if GINA cleared no malnutrition
- All cases performed with local surgeons – lower complexity used as teaching/training cases
- All cases managed by visiting Paediatric Anaesthetists (Italy and UK) with local anaesthetists in attendance
- Cleft teaching sessions (4 local Plastic surgeons covering North)
- Met local speech therapist lead
- Basic Surgical Skills session x2 for local medical students


Case Breakdown
| Surgical Cases at Shifa Hospital |
Age |
| Cleft soft palate |
8 months |
| Cleft soft palate |
2.5 Years |
| Cleft soft palate |
4 years old |
| Large anterior fistula (BCLP) |
2 years old |
| Unilateral lip revision & vomer flap |
2 years old |
| Lip revision + palate re-repair |
9 years |
| Unilateral lip revision |
19 years |
| Cleft soft palate |
3 years |
| Unilateral cleft lip & vomer |
6 months |
| Palate re-repair (BCLP) |
4 years |
| Cleft soft palate |
11 months |
| Cleft soft palate (VSD) |
10 months |
| Unilateral cleft lip revision |
16 years |
Hemi-nasal reconstruction
forehead flap, cartilage, septal hinge flap |
36 years |
| Cleft soft palate |
2.5 years |
| Cleft pharynoplasty (BCLP) |
24 years |
Rib recon septo-rhinoplasty *
large septal perforation, dorsal collapse (extra-corporeal septal reconstruction) |
26 years |
* Nasser Hospital final day

Issues Identified
| Issues |
Detail |
Plan/proposal |
| Cleft surgery backlog |
No cleft surgery for 2 years. |
Concentrate on primary surgery treatment/support and training |
| Poorly repaired clefts |
Visiting NGOs with likely very limited cleft experience. This is very difficult to regulate in the current heavily destroyed health infrastructure, particularly Field Hospitals. |
Proposal from Ministry of Health to make Shifa designated cleft centre. Any planned visiting cleft surgeons to work at Shifa with Dr Bassam local surgeon |
| Patient nutrition |
GINA support and monitoring
|
GINA support and monitoring
|
| Patient/family pre/post support |
GINA support and monitoring |
GINA outreach clinics – support families locally pre-post as transport very difficult |
| Surgical equipment & supplies |
Visiting teams/surgeons: severely restricted as very strict border crossing limitations
Local surgical instruments, sutures, supplies very limited and not cleft specific
|
Re-purpose existing instruments into ‘cleft trays’ Wait for restrictions to ease to allow regular supply and/or use of WHO containers |
| Anaesthetic Support & supplies |
No locally identified cleft specific Anaesthetist. Need same person(s) and need motivation/interest Severe lack of paediatric ET tubes, paediatric specific anaesthetic supplies. Currently all tubes are washed in a sink and re-used |
Visiting Paediatric Anaesthetist to ideally accompany visiting cleft surgeon to train/support local anaesthetic team |
| Cleft speech therapy support |
No local cleft trained speech therapist. Met Mousa Al Khardhee (head of local team of general SLTs). Mousa keen to collaborate |
Initial contact with West midlands cleft SLT team made remotely Visiting UK Cleft SLT much needed for future trips with Surgical team |
| No wider local Cleft MDT |
No cleft collaborative team |
Start with primary surgery, build in cleft speech support secondarily Build remote cleft MDT support with local surgeons |
| Unpredictable border approval |
For any visiting medic, final clearance to enter Gaza is made 24 hours before entry date. Medics can also be rejected at the border crossing. |
|
The table gives an overview of the key issues to building a sustainable cleft service. With a ceasefire in place, the overall number of acute war injuries has decreased. The local health ministry is trying to re-start all elective surgical services, though this is now with a shattered healthcare system and infrastructure.
Broadly, the following options were identified for cleft care options given the current restrictions and challenges:
- Option 1: wait for visiting missions only
- This option is unreliable, with no local sustainability
- Option 2: UK team to train local team to give independence
- concentrate on primary surgery, build in secondary speech surgery once primary established
- train/support/teach local SLT team in cleft speech
While in Gaza, and since returning to the UK, several cleft strategy conversations were made with CLEFT UK (Brian Sommerlad and Tim Goodacre), the local surgeons, Ahmed Mokhallati, and Andy Ferguson from IDEALS (UK based charity focusing on Ortho-plastic missions to Gaza). Andy was also in Gaza in December, and visited Shifa and Nasser Hospital.
Given the unpredictable approval and challenging situation, the current proposal is for small group of visiting UK cleft surgeons ideally with anaesthetic support to rotate visits on a 4-6 month basis with logistic and local support from IDEALS.

Conclusion
Despite the inherent difficulties the visit was extremely positive for both sides. The local surgeons appreciated being involved from the outset, and to be trained directly. Since the visit the two senior surgeons have started jointly operating with lower complexity cleft surgery independently, and remain in regular contact for advice.